ACLS (Advanced Cardiovascular Life Support) is a set of guidelines and skills. They are intended to manage serious cardiac and respiratory emergencies. ACLS is different from Basic Life Support (BLS). BLS involves CPR, basic airway management techniques, interventions such as electrocardiogram interpretation (ECG) interpretation, and advanced airway techniques. ACLS targets healthcare professionals dealing with critical situations directly.
ACLS certification was designed for healthcare providers working in acute or emergency care environments, including physicians, nurses, and paramedics. Certification demonstrates their ability to quickly recognize life-threatening situations while providing lifesaving care according to standard protocols that aim to maximize patient outcomes.
This guide explores the significance of ACLS and its skills and protocols as well as certification processes, as well as any difficulties experienced when applying ACLS in real-world settings.
ACLS: Importance
ACLS serves an integral function in healthcare due to its many advantages; with one sole goal in mind: increasing survival rates during critical situations.
Rapid response is key in mitigating an emergency situation and ACLS-certified providers have been specially trained to assess, diagnose, and treat emergencies quickly.
ACLS was designed around standardized protocols to guarantee patients receive consistent quality care wherever they seek it and reduce costs in doing so.
According to studies, ACLS increases patient survival and recovery rates significantly while leading to enhanced recovery results.
Communication and teamwork are critical during an emergency situation. ACLS emphasizes teamwork to enable all members of a group to effectively share information and make collective decisions together.
ACLS equips healthcare professionals with knowledge and tools that allow them to capitalize on every second during medical emergencies, helping make every moment count.
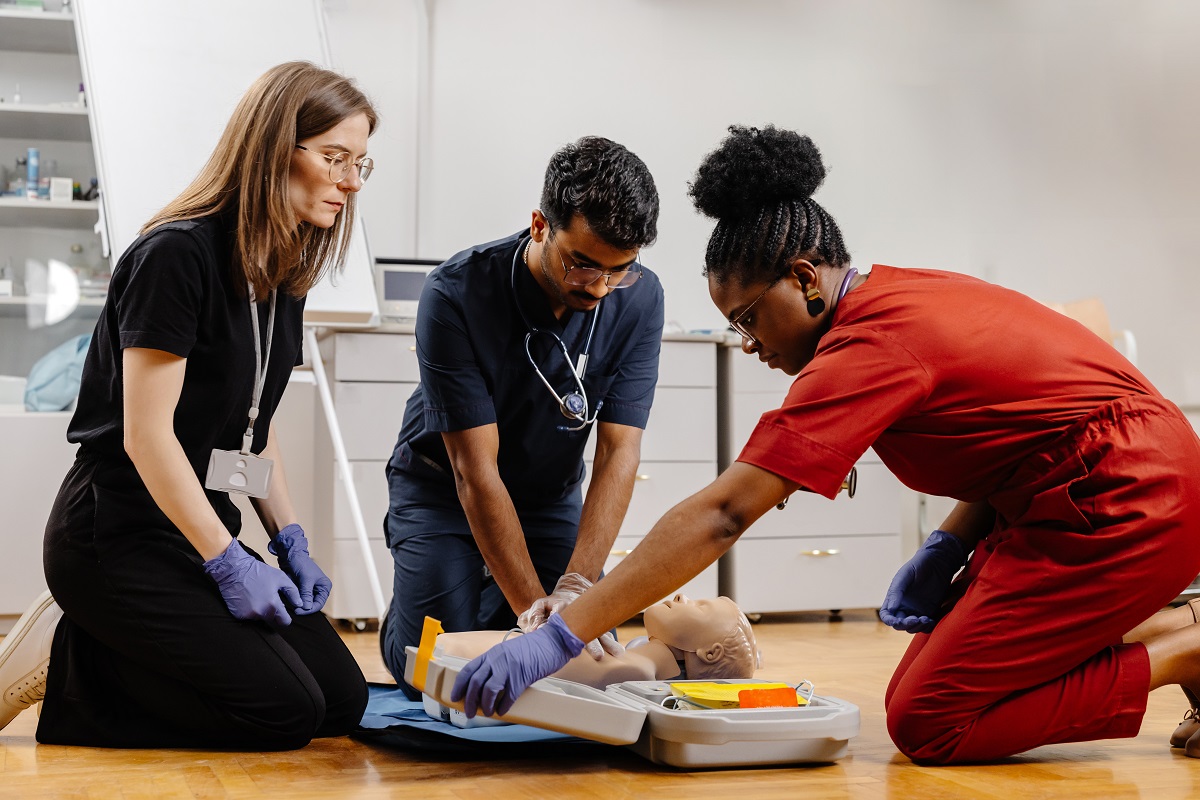
ACLS Training Components
ACLS training encompasses many techniques designed to save lives, from managing airways and administering medication. Each component of training has been specifically created to prepare providers for any situation that arises.
Airway Management.
ACLS centers around airway management. To ensure adequate oxygen reaches both the lungs and brain, maintaining an open airway is of utmost importance.
Key airway management techniques include: * Cleansing Methods (e.g. head tilt, chin lift, and jaw thrust) can help clear an unresponsive airway by means of basic clearance methods such as head tilting, chin lifting, and jaw thrust.
Bag-Valve Mask Ventilation – This technique employs an inflatable bag fitted with a mask attached to provide oxygen to patients who are having difficulty breathing, making this an essential skill in ACLS.
Advanced Airway Devices: When basic techniques fail, endotracheal intubation or supraglottic devices may provide the needed control over breathing that’s essential in respiratory distress or arrest situations.
Airway management is of critical importance in emergency care as it reduces hypoxia risk and protects brain oxygenation. Its
Chest Compressions & Circulation
ACLS relies on effective circulation management through chest compressions to keep blood circulating when the heart suddenly stops pumping, as part of their effective circulation management protocol:
Compression Depth and Rate: Providers have been instructed to apply pressure at 100-120 compressions per minute on the chest area. Defibrillation can help restore normal heart rhythm in cases such as ventricular fibrillation or pulseless ventricular Tachycardia.
Intravenous access may be provided when necessary. Common medications used include epinephrine, amiodarone, and lidocaine; their exact use will depend on each patient’s individual requirements.
Monitoring and Interpretation of Arrhythmias
ACLS provides essential diagnostic and therapeutic capabilities in diagnosing and treating arrhythmias. Healthcare providers learn how to recognize irregular heart rhythms that require attention as well as interpret them accurately.
Assessment of Rhythm Patterns and Trends: Conducting rhythm assessments can help assess whether the patient’s health is improving or declining, as knowing heart patterns helps make timely decisions. Knowing how to read rhythms accurately is crucial when managing cardiac patients.
Pharmacology for ACLS.
ACLS protocols would not be complete without medications to aid in stabilizing and managing cardiac emergencies. Each of the drugs prescribed under ACLS has its own role to play when stabilizing or managing cardiac emergencies. Epinephrine helps improve blood flow to stimulate heartbeat during cardiac arrest and promote cardiac recovery.
Amiodarone is an antiarrhythmic drug used to treat irregular heartbeats that could potentially be life-threatening. Lidocaine can also be used as an antiarrhythmic and Atropine is prescribed to increase heart rate in bradycardia cases.
Adenosine can help lower heart rates in cases of rapid heartbeats. Understanding its dosage, administration method, and potential side effects is essential in order to use medication correctly and avoid potential complications.
Post-Cardiac Arrest Care
ACLS should continue after spontaneous circulation has resumed; now its purpose shifts from stabilization to prevention of complications.
Monitor and support oxygen levels: After cardiac arrest, maintaining high levels of oxygen is crucial in order to prevent brain damage.
Arrhythmia detection: To protect against repeat heart events, monitoring cardiac activity continuously is key.
Blood Pressure Management: Stabilizing your blood pressure will lower the risk of strokes or cardiac arrest. Hypothermia protocols may be utilized in specific circumstances to protect the brain. Following emergency cardiac interventions, post-cardiac treatments ensure patients have every chance at recovering fully from their recovery process.
ACLS Algorithms
ACLS relies on algorithms that offer a structured care approach, and enable providers to manage different types and severity of emergencies with precision.
Pulseless Algorithm
This algorithm is critical in cases of cardiac arrest without a pulse; its steps include:
CPR Start-Up: High-quality CPR should be initiated quickly to maintain circulation, with defibrillation used when certain arrhythmias have been identified and Epinephrine administered every 3 to 5 minutes during CPR to stimulate the heart.
Antiarrhythmic Drugs: Amiodarone and lidocaine may be effective at controlling irregular heartbeats.
Bradycardia Algorithm
This algorithm addresses symptoms by measuring pulse rates instead of heart rates directly.
Monitoring for Instability – Providers will observe symptoms such as dizziness and fatigue to detect instability. Atropine Administration Atropine can be prescribed to increase heart rate when bradycardia symptoms arise, whilst transcutaneous Pacing should only be considered if medication doesn’t work effectively enough.
Tachycardia using Pulse Algorithm
An elevated heart rate with a pulse requires careful observation and treatment depending on how stable the individual is. When unstable patients require immediate intervention, Adenosine administration may also be administered as part of treatment to assist in stabilizing them.
Synchronized Cardioversion: For patients who exhibit an unstable rhythm, an electric shock may be used to restore it to its usual pattern.
Acute Coronary Syndrome Algorithm
ACS refers to the management of heart attacks and similar conditions with the aim of limiting damage to cardiac muscle as much as possible.
Aspirin and Nitroglycerin Administration: These medications relieve symptoms while also increasing circulation. ECG Interpretation – ECGs can be used to analyze the severity and type of heart events.
Advanced Medical Treatment: Additional treatment, such as Percutaneous Coronary Interventions (PCI), may be necessary. With these algorithms in place, chances of a positive outcome increase significantly by making sure the necessary steps are taken as quickly as possible.
ACLS Certification
ACLS certification can be a requirement in emergency and acute care settings, verifying healthcare providers’ ability to deliver timely and effective care in critical circumstances.
In order to become certified, providers must complete an ACLS structured course which includes:
BLS Certification Required Prior to ACLS Training: In order to enroll in ACLS courses, Basic Life Support certification is a precondition.
The Theory and Skills Assessment is an in-person training program covering airway management, drug administration, and ACLS protocols. Candidates must pass both written and practical assessments to pass this examination.
Recertification
ACLS certification must be renewed every two years to maintain skills and knowledge, keeping up-to-date on updates and protocols of cardiac emergency care services. Recertification classes provide this opportunity.
ACLS Latest Guidelines
The American Heart Association (AHA), using research-driven updates, regularly revises ACLS guidelines. Recent changes emphasize minimizing interruptions to chest compressions, providing high-quality CPR, and updating medication protocols – so providers must keep abreast of changes so their skills stay current.
Conclusion
ACLS certification is an indispensable skill for healthcare professionals working in high-stakes environments, with its structured approach to cardiac and respiratory emergencies providing immediate evidence-based treatments that could save lives. ACLS-trained professionals have proven invaluable as part of critical care teams.