Every patient matters. But in healthcare, some needs simply cannot wait. A blocked airway, severe bleeding, or sudden cardiac arrest must be addressed immediately — not because one patient is more valuable than another, but because the body has critical functions that must stay intact for survival.
This is the true meaning of prioritizing patients: responding to needs in the right order, so every individual receives safe, effective, and timely care. From hospital emergency rooms to everyday settings where CPR is performed, prioritizing patient care ensures that no second is wasted and no need is overlooked.
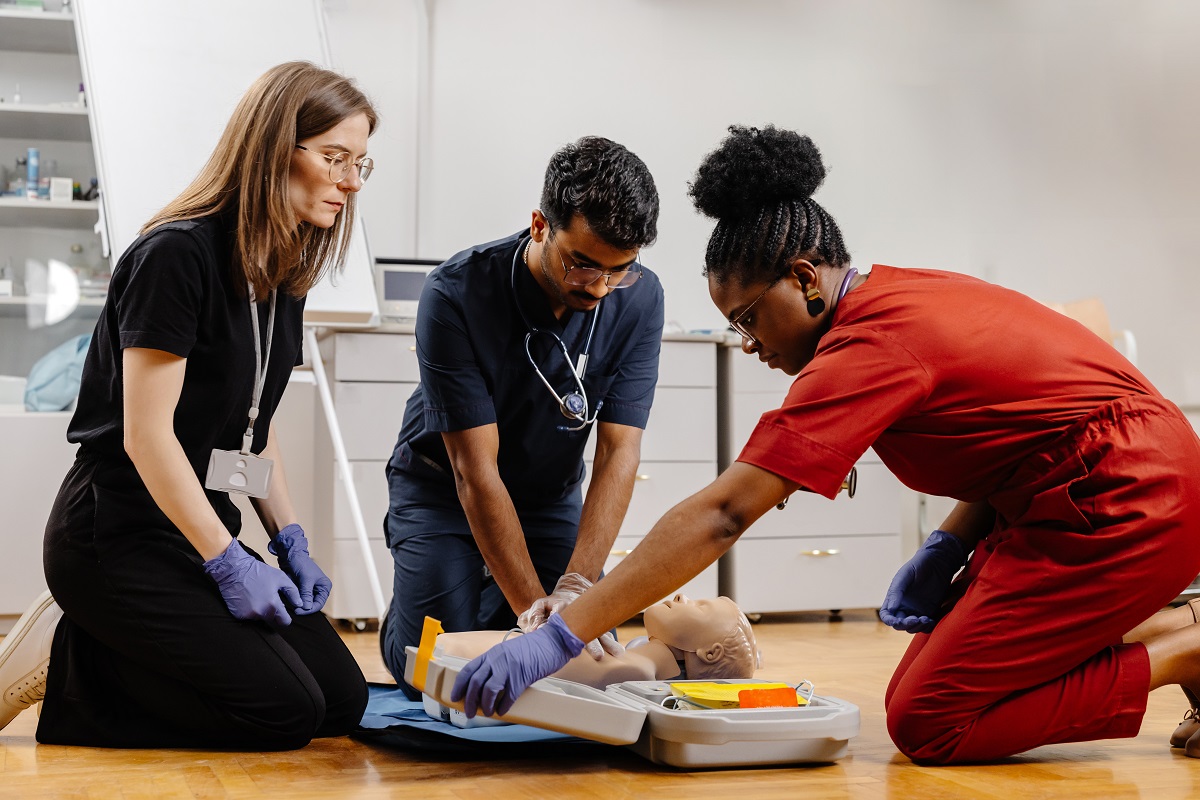
In this blog, we’ll explore a clear process anyone can follow to recognize and respond to the priority needs of patient care. You’ll see how professionals use structured steps to assess, act, and reassess — and how CPR and BLS training can prepare you to do the same in critical moments.

Key Takeaways
- Prioritizing patients means addressing urgent needs first, not valuing one patient over another.
- Every patient is important — the order comes from the urgency of their condition.
- CPR and BLS training provide practical steps to act quickly and correctly in emergencies.
- Proper prioritization improves safety and outcomes for all patients.
Assess Immediate Life Threats
When someone collapses or suddenly becomes unresponsive, most people freeze. The mind races with questions: Do I call for help first? Should I check for a pulse? What if I make a mistake? These are natural thoughts — and exactly why learning the proper order of response is so important.
The foundation of prioritizing patients begins with what professionals call the ABCs: Airway, Breathing, Circulation. These three functions are the body’s most basic requirements for life. If one is missing, everything else — even serious injuries like broken bones — must wait.
- Airway: If the airway is blocked, no air can reach the lungs. This is why checking if the person can speak, cough, or breathe is always the first step. Something as simple as tilting the head back to open the airway can make the difference between life and death.
- Breathing: Even with a clear airway, breathing may still be absent. This is when CPR skills become essential. If someone is not breathing normally, immediate chest compressions give the brain and heart the oxygen they desperately need.
- Circulation: Without circulation — the pumping of blood through the body — oxygen cannot reach vital organs. Severe bleeding or a heart that has stopped must be managed right away.
You may wonder, why this order? Why not treat bleeding first, or rush to call an ambulance? The answer is simple: the body only survives minutes without oxygen. That’s why airway and breathing always come before anything else. A study from Medline Plus highlights how following this sequence consistently leads to better survival rates in emergencies.
It isn’t about choosing one patient over another — it’s about addressing the most urgent function in order so every patient has the best chance at recovery.
This structured process is taught in CPR and Basic Life Support (BLS) courses. These trainings give people the confidence to act, not guess. They turn panic into purpose by teaching you exactly how to prioritize patient care when seconds count. Imagine being at a family gathering and someone suddenly collapses. Without training, hesitation takes over.
With training, you know exactly what to do first: check for responsiveness, open the airway, assess breathing, and begin compressions if needed.
In hospitals, providers use the same steps. Learning how to prioritize patients in hospitals doesn’t only apply to professionals in scrubs; it applies to anyone who may face an emergency at work, at school, or at home. And here’s the important truth: emergencies rarely give you time to think — they demand action. The ABCs give you a safe, proven order to follow, so you don’t have to guess what comes next.
By starting with airway, breathing, and circulation, you meet the most critical patients’ needs first. It creates a clear level of response, ensures that no step is skipped, and lays the foundation for everything else that follows in health care.
Identify Urgent vs. Non-Urgent Needs
Once airway, breathing, and circulation are under control, the next step in prioritizing patients is deciding which problems require rapid attention and which can safely wait. This is not about choosing who matters more — it’s about recognizing which conditions could worsen quickly if left untreated.
For example:
- A person who is alert but has a broken arm can usually wait until life-threatening issues are handled.
- A patient with severe bleeding or signs of shock must be treated immediately.
- Someone with chest pain and difficulty breathing may not look as critical as bleeding, but the condition could signal a heart attack and needs urgent care.
This process is the foundation of prioritizing patient care. Hospitals use it daily through triage systems, where patients are seen not by arrival time but by the seriousness of their condition.
At Comfi-Kare CPR, we provide BLS (Basic Life Support) courses that teach how to recognize these urgent “red flags.” Participants learn to identify critical warning signs such as:
- Severe or uncontrolled bleeding.
- Symptoms of stroke (slurred speech, weakness, facial droop).
- Sudden chest pain or shortness of breath.
- Loss of consciousness.
These skills give responders the confidence to act quickly, applying care in order of urgency while waiting for advanced medical help. Even outside the hospital, knowing how to prioritize patients in hospitals and in community emergencies makes a measurable difference in outcomes.
When urgent needs are separated from non-urgent ones, the effects in health care are clear: patients are stabilized before conditions worsen, providers manage their resources more effectively, and everyone receives care that is appropriate to their level of need.
Reassess and Adjust Priorities Continuously
Prioritizing patients is not a one-time decision. A person’s condition can change in minutes, which means what was stable a moment ago can suddenly become critical. Continuous reassessment is what keeps care safe and effective.
For example, a patient who initially had normal breathing may begin to struggle, or someone who appeared alert could become disoriented as shock develops. Without frequent checks, these changes can be missed — and the opportunity for timely intervention is lost.
Healthcare providers follow a cycle: assess, act, reassess. This method ensures that the most urgent problems remain at the top of the list, while less urgent needs are addressed when it is safe to do so. According to MedlinePlus, regular monitoring during emergencies is essential because symptoms can progress quickly even after initial treatment.
This principle applies outside the hospital, too. In CPR and BLS scenarios, responders are taught to check frequently for changes in breathing, pulse, or responsiveness while providing care. You can contact us at Comfi-Kare CPR directly for information about our CPR and BLS courses, which explain these steps in detail and prepare you to act with confidence in real emergencies.
Reassessment also prevents one common mistake: focusing on a single issue and overlooking new problems. For instance, it is natural to keep attention on a bleeding wound, but if the patient’s breathing becomes shallow during treatment, priorities must shift back to airway and breathing first.
By reassessing regularly, you protect the health of the patients in a way that is safe, structured, and adaptable. It keeps care aligned with real-time needs, reduces errors, and strengthens trust between patients and those providing care.
Tips and Questions to Ask When Prioritizing Patients
Emergencies don’t come with instructions, but a structured way of thinking makes it easier to respond. Use these tips and guiding questions to stay focused and meet patients’ needs in order of urgency.
Practical Tips
- Stay calm and observant. Panic clouds judgment — steady focus allows you to act in the right order.
- Follow the ABCs (Airway, Breathing, Circulation). This sequence always guides first actions.
- Check for red flags. Severe bleeding, chest pain, slurred speech, or sudden collapse demand immediate care.
- Use clear communication. If others are present, direct them with simple instructions: “Call 911,” “Get the AED,” “Hold pressure here.”
- Reassess often. Patients can change quickly — stability one minute doesn’t mean stability the next.
Key Questions to Ask Yourself
- Is the patient breathing normally?
- Do I see signs of severe bleeding or shock?
- Has the patient’s condition changed since my last check?
- Does this problem need immediate attention, or can it wait safely?
Questions to Ask the Patient (When Possible)
Sometimes urgent needs show through mental changes or confusion rather than physical signs. Asking simple questions helps uncover hidden problems:
- Can you tell me your name? (tests orientation — confusion may signal a serious issue).
- Do you know where you are right now?
- Are you feeling dizzy, weak, or in pain?
- When did this start? (helps understand timing and urgency).
By combining physical checks with simple questions, you get a clearer picture of the patients’ needs. This balanced approach makes prioritizing patient care more accurate and ensures that nothing important is missed, which is also a key principle in effective nursing practice.
Conclusion
At its core, prioritizing patients means giving attention to the most urgent needs first so that every individual receives safe and effective care. Whether it’s restoring breathing, stopping bleeding, or noticing sudden changes in awareness, the process provides a clear order of action when time matters most.
These principles extend beyond hospitals. They are the same steps practiced in CPR and BLS training, where everyday people learn how to respond confidently in emergencies. By understanding the priority needs of patient care, you not only support recovery — you also create stronger outcomes and reduce the risks that come with hesitation.
If you’d like to be prepared to act in real situations and gain skills that make a difference, call Comfi-Kare CPR today at 240-676-4239. Our team will provide you with information about upcoming courses and help you take the first step toward being ready when it matters most.
Frequently Asked Questions about Prioritizing Patients
How do you prioritize your patients?
Patient prioritization means addressing the most urgent needs first — usually following the ABCs: airway, breathing, and circulation. This ensures life-threatening issues are handled before less critical concerns.
What is it called when you prioritize patients?
This process is often called triage, a method used in hospitals and emergency care to decide the order of treatment based on urgency, not on who arrived first.
What is a method of prioritizing treatment of patients?
A common method is the step-by-step ABCs approach combined with continuous reassessment. This helps healthcare providers and responders focus on the priority needs of patient care in order of severity.
What are the ABCs of prioritization?
The ABCs stand for Airway, Breathing, and Circulation, and they are the foundation of patient prioritization. This method places patient safety first by ensuring that life-threatening issues are addressed before less urgent needs.
What is the first priority for a patient?
The first priority is always to make sure the patient has an open airway and is able to breathe. Without oxygen, survival is only possible for a few minutes, which is why airway and breathing are managed before any other care.